

Review of the history of the patient showed that he was diagnosed six years ago with Behçet’s disease (BD). The diagnosis was made according to International Criteria for Behçet’s Disease based on the combination of oral and genital ulcers and acneiform lesions. He was treated with colchicine for recurrent oral and genital ulcers.
The diagnosis of BD, the inflammatory activity in his blood tests, and the CT interpretation by the radiologist suggested a pulmonary artery aneurysm in the left inferior lobe which was partially thrombosed. Other causes of haemoptysis particularly, tuberculosis, pulmonary malignancies, and anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis were considered unlikely. Screening of tuberculosis in sputum samples was negative, CT showed no signs suggestive of pulmonary malignancies and myeloperoxidase anti-neutrophil cytoplasmic antibody (MPO-ANCA) and proteinase 3 (PR3)-ANCA were both negative.
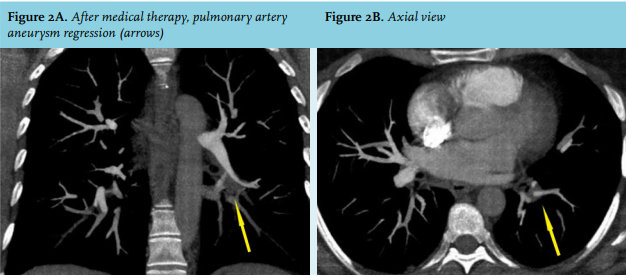
Intravenous methyl prednisolone 1 g/d for three days followed by oral prednisone 60 mg/d (1 mg/kg/d) was administered; the prednisone dose was subsequently tapered. Concomitantly, cyclophosphamide at a dose of 15 mg/kg was given every four weeks over six months and then switched to oral azathioprine (3 mg/kg/d). Within one month, haemoptysis disappeared and six months later, a chest CT showed resolution of the pulmonary aneurysm and thrombosis (figure 2A, B).
Pulmonary artery aneurysm is a life-threatening condition. Congenital vascular diseases are the main etiology. Others causes include infections, mainly tuberculosis and syphilis, pulmonary arterial hypertension, and chronic pulmonary embolism. BD can cause inflammation of the pulmonary arteries that result in aneurysms. Surgical or endovascular therapies are the commonly used treatment options for pulmonary artery aneurysm.
Our case illustrates the importance of considering the etiology of an arterial aneurysm before choosing the treatment option. Vascular surgery in BD is associated with a high risk of occlusion, recurrence, and false aneurysm formation.1 Medical therapy combining corticosteroid and immunosuppressive agents should be considered in patients with arterial aneurysm due to BD.2 No consensual treatment of pulmonary artery aneurysms caused by BD has been developed; the most commonly administered therapy is corticosteroid combined with cyclophosphamide pulses.3 In refractory cases, anti-tumour necrosis factor should be considered4 and surgery is discouraged due to the high risk of complications.4 In our patient, a therapy consisting of combined corticosteroid and cyclophosphamide pulses followed by a switch to oral azathioprine therapy was effective.
DISCLOSURES
All authors declare no conflicts of interest. No funding or financial support was received.
REFERENCES