Full textPDF
Full text
CASE REPORT
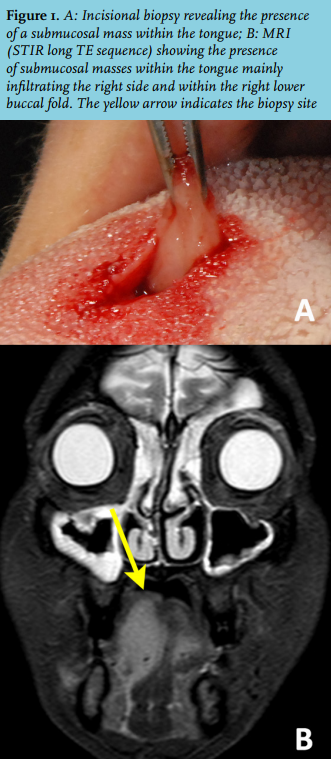
A 56-year-old female came to our hospital complaining of a relapsing-remitting swelling on the right side of the tongue, dyspnoea and bronchitis not responding to antibiotic therapy. Five years before she had been diagnosed with chronic leucocytosis: blood tests showed hyper-eosinophilia and immunophenotyping of peripheral blood showed positivity of CD3, CD4, CD2, CD7, CD10, CD52, thus suggesting a lymphoproliferative disorder. The patient refused to proceed with further investigations. At admission, due to her past medical history, a bone marrow biopsy, magnetic resonance imaging (MRI) with contrast medium of the head and neck and serum protein electrophoresis were performed. Bone marrow biopsy detected cell monoclonality on a background of polyclonal T-cells, but was not able to identify any neoplasia, while serum protein electrophoresis disclosed a high level of gamma proteins. MRI highlighted three submucosal masses: one of the right body of the tongue, another one in the left anterior part of the tongue and the last one in the right oral vestibule, so that the patient was referred to the oral medicine clinic. Clinical examination just revealed an asymptomatic swelling of about 2-3 cm in diameter involving the right side of the tongue with an overlying healthy mucosa and a doughy consistency. An incisional biopsy confirmed the presence of a soft yellowish mass infiltrating the tongue (figure 1).
WHAT IS YOUR DIAGNOSIS?

