Full textPDF
Full text
CASE REPORT
A 30-year-old male with no known medical history presented to the emergency department with a one-week history of polyuria, polydipsia, weakness, and weight loss. This was associated with a significantly decreased appetite and two episodes of vomiting over the two days prior to hospital presentation. On admission, he was obtunded, hypothermic at 34.2° C, with a blood pressure 90/53 mmHg, heart rate 116 beats/min and respiratory rate 33 breaths/min. He was lethargic, emaciated, and had dry mucous membranes. Physical examination was also significant for crepitus over the neck and shoulders. Laboratory studies were as follows: white blood cell 18.8 k/ µl (3.8-10.6 k/µl), glucose 1182 mg/dl (50-140 mg/dl), beta hydroxybutyrate 14.79 mmol/l (0.00-0.30 mmol/l), blood urea nitrogen 53 mg/dl (10-25 mg/dl), creatinine 4.37 mg/dl (< 1.13 mg/dl), glycated haemoglobin 12.3% (< 5.7%), arterial pH 6.94 (7.35-7.45), and arterial bicarbonate 1.5 mmol/l (22-26 mmol/l).
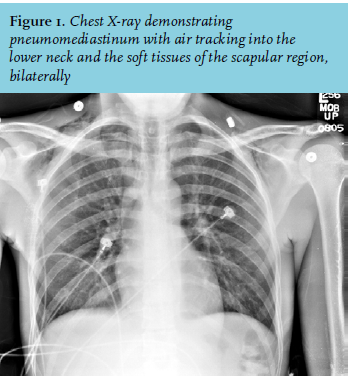
The electrocardiogram demonstrated sinus tachycardia. Chest X-ray showed air tracking into the soft tissue of the lower neck and bilateral scapular regions without pneumothorax (figure 1).
WHAT IS YOUR DIAGNOSIS?