Full textPDF
Full text
CASE REPORT
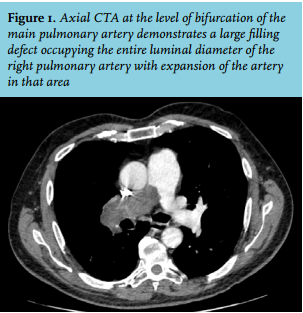
A 72-year-old man presented with progressive dyspnoea and weight loss for two months. He had a 20 pack-year tobacco history. He had not travelled recently. Vital signs were significant for a tachycardia of 102 beats/minute and an oxygen saturation of 95% on room air. The jugular venous pulse was elevated. Cardiopulmonary examination was normal. He had minimal lower extremity oedema. Laboratory evaluation revealed only mild normocytic anaemia. Brain natriuretic peptide was 54 ng/l. A clear chest radiograph prompted computed tomography angiography (CTA) of the chest (figure 1).
WHAT IS YOUR DIAGNOSIS?

