

INTRODUCTION
The effect of thrombosis prophylaxis on prevention of symptomatic venous thrombosis for two of the most commonly performed orthopaedic treatments world-wide (lower leg cast immobilisation and arthroscopy of the knee) is not well established.1-14 With this survey study we aim to provide insight into the thrombosis prophylaxis policies of orthopaedic and trauma surgeons, the relevant indications, and the considerations for providing such therapy.
Venous thrombosis (i.e. deep vein thrombosis and pulmonary embolism) occurs in about 1-2 per 1000 persons per year in the general population and is a serious condition leading to chronic morbidity (e.g. post-thrombotic syndrome and pulmonary hypertension) and an increased mortality.15-19 The risk of venous thrombosis is increased after surgery, and is particularly high after orthopaedic surgery (estimated 4% in 35 days after major orthopaedic surgery).3,20,21 Because of this high risk, thrombosis prophylaxis is recommended for these patients.3,4,8 However, most trials investigating patients with lower leg cast immobilisation and knee arthroscopy were underpowered, included patients at additionally high risk for venous thrombosis (i.e. complete leg cast immobilisation, ligament reconstructions), or used asymptomatic venous thrombosis as the primary endpoint.1-14 For these reasons, most national and international guidelines advise against thrombosis prophylaxis for these patients while others recommend instead the use of prophylaxis only in patients with an increased risk for venous thrombosis (e.g. longer duration/more extensive surgery or in patients with additional risk factors) or leave it to the clinician to decide whether to provide prophylactic treatment.3,4,8
Despite the lack of an evidence base and ambiguous guidelines, 70% of orthopaedic and trauma surgeons provided thrombosis prophylaxis to patients with lower leg cast immobilisation and 71% of orthopaedic surgeons did so for patients who underwent knee arthroscopy in the Netherlands in 2007.22 The reasons behind this large-scale use of thrombosis prophylaxis are unknown.22-24 Clinical experience suggests that the proportion of surgeons providing prophylaxis to these patients has increased since 2007. Therefore, the aim of this survey study was to obtain insight into the thrombosis prophylaxis policies and rationales of orthopaedic and trauma surgeons for patients with lower leg cast immobilisation and those undergoing arthroscopy of the knee.
MATERIALS AND METHODS
 |
In July 2013, a digital survey (NetQuestionnaires, version 6.0, NetQuestionnaires Netherlands B.V, Utrecht, the Netherlands) was sent to all departments of orthopaedic surgery (90 hospital departments and 16 private orthopaedic clinics) and all departments of surgery (89 hospital departments*) in the Netherlands. The survey concerned thrombosis prophylaxis policy in patients with lower leg cast immobilisation and patients undergoing arthroscopy of the knee. Careful attention was put into designing unambiguous and non-leading questions and response choices.25,26 A copy of the survey (in Dutch) is available as supplement material. A link to the survey was included in a personalised email sent on behalf of the heads of the (sub)departments of orthopaedic surgery and trauma surgery (RGHHN and IBS) of the Leiden University Medical Center. The survey was sent to one orthopaedic surgeon and one trauma surgeon for every hospital department or private clinic. Trauma surgeons were selected based on their registration as trauma surgeons and orthopaedic surgeons based on their registration as orthopaedic surgeons and/or lower extremity or knee surgeons. Surgeons who did not respond promptly were sent two reminders before another orthopaedic or trauma surgeon from the same department was contacted.27 For orthopaedic surgeons working in hospitals, the survey regarded the thrombosis prophylaxis policy in patients with lower leg cast immobilisation and those undergoing arthroscopies of the knee. For orthopaedic surgeons working in a private clinic, only questions regarding arthroscopy of the knee were included. Trauma surgeons were asked about the thrombosis prophylaxis policy in patients with lower leg cast immobilisation.
All data were analysed anonymously using SPSS version 20.0.0 (IBM, Armonk, New York, US). For knee arthroscopy, the results of the hospital departments and orthopaedic private clinics were combined as these results were similar. For lower leg cast immobilisation, the data were separately analysed for orthopaedic and trauma surgeons. Answers to open questions were categorised. Categorical data were expressed as proportions using percentages.
RESULTS
The survey was completed in 93 of the 106 contacted departments of orthopaedic surgery (79 hospital departments (88%) and 14 orthopaedic private clinics (88%)). Trauma surgery departments had a response rate of 81% with 72 of 89 departments completing the questionnaire. Of these departments, 69 (96%) trauma surgery and 70 (89%) orthopaedic surgery departments had protocols concerning thrombosis prophylaxis in patients with lower leg cast immobilisation while 84 (90%) orthopaedic surgery departments had thrombosis prophylaxis protocols for knee arthroscopy patients. The majority of these protocols were based on the guidelines of the Dutch Institute for Healthcare Improvement (CBO) (table 1).
Thrombosis prophylaxis
 |
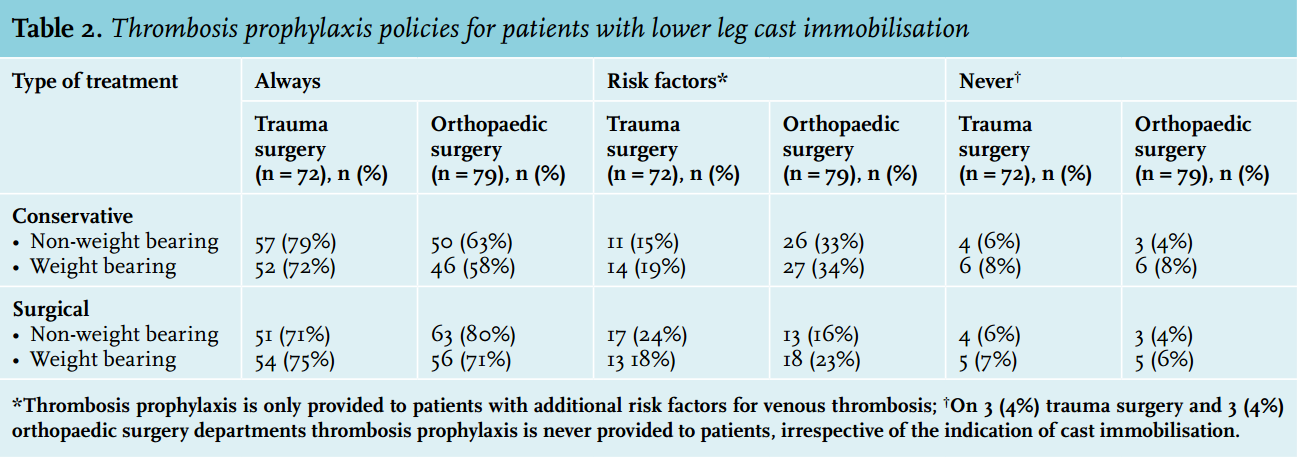
Thrombosis prophylaxis for patients with lower leg cast immobilisation is certainly the norm with only 3 of the 72 (4%) trauma surgery departments and 3 of the 79 (4%) orthopaedic surgery departments opting against the practice. The remaining departments base the decision on whether or not to give thrombotic prophylaxis upon patients’ ability to bear weight, the presence of risk factors, and type of surgical intervention (table 2). Knee arthroscopy patients never receive prophylactic treatment at 10 (11%) of the 93 orthopaedic surgery departments. In departments that do provide prophylactic therapy, the decision to prescribe prophylaxis is highly dependent on the indication for knee arthroscopy (table 3). Further, for both indications, the decision to give prophylactic treatment is dependent on the presence of additional risk factors for venous thrombosis, the presence of risk factors for bleeding and the use of co-medications that influence the coagulation system, such as non-steroidal anti-inflammatory drugs and platelet aggregation inhibitors. Surgeons that provide prophylaxis only to patients with additional risk factors do so predominantly for the following risk factors: previous episode of venous thrombosis (22 (96%) of trauma surgeons and 61 (90%) of orthopaedic surgeons); family history of venous thrombosis or hereditary thrombophilia (18 (96%) of trauma surgeons and 45 (66%) of orthopaedic surgeons); obesity (BMI ≥30) (17 (74%) of trauma surgeons and 28 (41%) of orthopaedic surgeons); hormonal contraception use (14 (61%) of trauma surgeons and 31 (46%) of orthopaedic surgeons).
Type of thrombosis prophylaxis
The prophylactic treatment of choice for patients with lower leg cast immobilisation is low-molecular-weight heparin (LMWH) at 67 trauma surgery departments (97%) and 74 orthopaedic surgery departments (97%). The most commonly used LMWH is nadroparin. LMWH is used in all (83 (100%)) of the orthopaedic surgery departments providing prophylaxis with the most common choice again being nadroparin.
Duration of prophylaxis
In patients with lower leg cast immobilisations, prophylactic treatment is almost always provided for the duration of immobilisation (trauma surgery departments 66 (96%) and orthopaedic surgery departments 68 (89%)). At the other departments, prophylaxis is provided during hospital stay, for a fixed period of time, or for the period of cast immobilisation plus one week thereafter. For knee arthroscopy patients the duration of prophylaxis ranges from one day to six weeks and strongly depends on the indication for the knee arthroscopy. Further, the duration of prophylactic treatment per indication varies widely between hospitals (figure 1).
Reasons for thrombosis prophylaxis
Rationales for the prescribing of prophylactic therapy include the assumption that the reduction in risk of thrombosis outweighs the associated increased bleeding risk, that some individual clinical experience suggests prophylaxis is effective, and that clinicians are acting in accordance with their department or hospital protocol (table 4).
Choice for type of thrombosis prophylaxis
 |
The most prevalent reason for LMWH as prophylactic treatment of choice in patients with lower leg cast immobilisation is that this action is in accordance with hospital or department protocol in 54 trauma surgery (81%) and 57 orthopaedic surgery departments (77%). In addition, in 28 trauma surgery (42%) and 29 orthopaedic surgery departments LMWH is considered the safest prophylactic treatment, in 19 (28%) trauma surgery and 29 (39%) orthopaedic surgery departments it is preferred because of extensive clinical experience and in 15 trauma surgery (22%) and 14 orthopaedic surgery departments (19%) it is considered to be the most effective prophylactic treatment. The rationales for the preference for LMWH as prophylactic treatment prior to knee arthroscopies are varied. The use of LMWHs is in accordance with the department or hospital protocol at 49 (59%) departments; LMWHs are considered the safest option at 47 (57%) departments; LMWHs are considered to be the most effective option at 28 (34%) departments and at 25 departments (30%) LMWHs are preferred because of extensive clinical experience with this type of anticoagulants.
DISCUSSION
In this survey study, we were able to give a detailed overview of current thrombosis prophylaxis policies in the Netherlands for patients with lower leg cast immobilisation and for patients who had a knee arthroscopy. Despite insufficient evidence on the effect of prophylaxis on the prevention of symptomatic events and on its cost-effectiveness, prophylaxis seems to be prescribed in the large majority of clinical practices. Further, substantial differences exist in prophylactic strategies between departments depending on the indication for below-knee cast immobilisation or knee arthroscopy and on the presence of additional risk factors for venous thrombosis. The most important reasons for providing prophylactic treatment as indicated by respondents were the assumption that the risk reduction for thrombosis outweighs the bleeding risk; that clinicians have the experience that prophylaxis is effective; and that clinicians act in accordance with department or hospital protocol by providing prophylaxis.
In trials regarding thrombosis prophylaxis in patients with below knee cast immobilisation or undergoing knee arthroscopy, asymptomatic venous thrombosis has generally been used as a primary endpoint. The incidences of these events in the trials’ control groups varied between 0-15.6% for knee arthroscopy (follow-up 1 week to 3 months) and between 4.3-36% during 4-6 weeks of cast immobilisation.1,2,5-7,9-14 However, these trials were underpowered to draw conclusions on the prevention of symptomatic venous thrombosis as the risks of these events were much lower (between 0-2.5% for knee arthroscopy and 0-5.5% for cast immobilisation).3,4,8 The risks of these symptomatic events are further not representative for below knee cast immobilisations and regular knee arthroscopies because of the inclusion of patients with more extensive trauma or surgery (complete leg cast and ligament reconstructions) for whom the expected risk of venous thrombosis is higher.28-32 Because of this, a balance between the benefit (prevention of symptomatic events) and risk of complications, such as bleeding events, cannot be established here.

This lack of evidence is reflected in the variation among guideline recommendations. The guideline of the American College of Chest Physicians recommends no prophylaxis while the guideline of the National Institute for Clinical Excellence (United Kingdom) recommends considering prophylaxis in the presence of additional risk factors.3,4 Further, the guideline of the CBO gives no definite recommendation for patients with lower leg cast immobilisation. For knee arthroscopy in general it recommends no prophylaxis; however, for reconstructive surgery or in patients with additional risk factors prophylaxis can be considered.8 Considering that the majority of department protocols are based on the CBO guideline, the variation in treatment strategies in the Netherlands may be explained by the fact that these guidelines can be interpreted in several ways, which is again due to the lack of evidence in the literature.
In comparison with previous survey studies, there seems to be a further increase in the use of thrombosis prophylaxis. For lower leg cast immobilisation, the proportion of departments where prophylaxis is never prescribed further decreased from 50% in 2002 and 30% in 2007 to only 4% in 2013.22-24 For knee arthroscopy the proportion of departments that never use prophylaxis decreased from 40% in 2002 and 48% in 2007 to 11% in 2013.22,23 In addition, there are international differences. For example, in the United Kingdom in 2010, only 16% of the orthopaedic surgery departments routinely provided prophylaxis to patients with lower leg plaster casts.33 In Italy, as early as 2004, 94% of orthopaedic surgery departments were providing thrombosis prophylaxis for knee arthroscopy.34
When interpreting our results, some limitations need to be taken into account. In this study, we assessed the prophylaxis policies at department but not at the individual physician level. The response of the single individual surgeon does not necessarily represent that of the department. However, the vast majority of orthopaedic surgery departments (89% for lower leg cast immobilisation and 90% for knee arthroscopy) and trauma surgery department (96%) have a protocol regarding thrombosis prophylaxis in these patients. We expect that any variation within departments will therefore be small. Furthermore, the response rate of our study is not 100%. However, our response rates of 81% and 88% are still high and well above the 70% needed to limit non-response bias.35,36 In addition, a non-validated survey was used. Furthermore, as in most survey studies, there is a risk of the respondent answering what he or she feels is appropriate rather than true. Because of this, particular attention was put into the design of non-leading and unambiguous questions and answer options.25,26
While we can only speculate about possible explanations for the recent further increase in the use of thrombosis prophylaxis, it could be that defensive medicine has become more predominant over evidence-based medicine. However, the large-scale use of thrombosis prophylaxis without a proper scientific basis for a beneficial effect may have medico-legal implications for involved clinicians, especially when (bleeding) complications occur. Although the bleeding risk with LMWH is perceived to be low, the absolute number of bleeding events can be high since both knee arthroscopy and lower leg cast immobilisations are frequently performed procedures.
Our results indicate that there is a clear need for high-quality research on this topic. Uniform evidence-based prophylactic treatment across hospitals is needed in order to improve the quality of care of patients. Instead of focusing on asymptomatic venous thrombosis, the primary endpoint of new studies should be symptomatic venous thrombosis.3,30 In addition, complications of prophylactic therapy, such as bleeds, need to be taken into account in order to establish a benefit-risk ratio. As for cast immobilisations, only patients with lower leg cast immobilisations should be included while for knee arthroscopy there is a need for trials with better stratification in terms of arthroscopy type.30 Further, identification of high-risk groups is needed, which can lead to individualised prophylactic therapy in order to optimise the benefits and risks from anticoagulant therapy.3
CONCLUSION
Based on this questionnaire study it seems that thrombosis prophylaxis is given to patients with lower leg cast immobilisation and around knee arthroscopies at the large majority of orthopaedic and trauma surgery departments in the Netherlands, despite insufficient evidence for a beneficial effect. In addition, large variations in prophylaxis strategies appear to exist between departments for different types of indications for lower leg cast immobilisation and arthroscopy of the knee. Uniform prophylactic treatment across hospitals, based on good quality evidence, is needed to improve the quality of care of these patients.
ACKNOWLEDGEMENTS
We would like to thank all trauma and orthopaedic surgeons who completed the questionnaire, P.V.D. Malhoe and I. de Jonge for their help with digitalising the questionnaire and N. Saadah for his critical appraisal of the language.
DISCLOSURES
Funding: This research project is part of a project funded by ZonMw (grant number 171102001): The funding source had no role in the design and conduct of the study; in the collection, analysis and interpretation of the data; or in the preparation, review, or approval of the manuscript
Conflicts of interest statement: Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/ licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
REFERENCES
1. Camporese G, Bernardi E, Prandoni P, et al. Low-molecular-weight heparin versus compression stockings for thromboprophylaxis after knee arthroscopy: a randomized trial. Ann Intern Med. 2008;149:73-82.
2. Canata GL, Chiey A. Prevention of venous thromboembolism after ACL reconstruction: a prospective, randomized study. ISAKOS (International Society of Arhtroscopy, Knee Surgery and Orthopaedic Sports Medicine). 2003;Poster 71.
3. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e278S-325S.
4. Hill J, Treasure T. Reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to hospital: summary of the NICE guideline. Heart. 2010;96:879-82.
5. Jorgensen PS, Warming T, Hansen K, et al. Low molecular weight heparin (Innohep) as thromboprophylaxis in outpatients with a plaster cast: a venografic controlled study. Thromb Res. 2002;105:477-80.
6. Kock HJ, Schmit-Neuerburg KP, Hanke J, Rudofsky G, Hirche H. Thromboprophylaxis with low-molecular-weight heparin in outpatients with plaster-cast immobilisation of the leg. Lancet. 1995;346:459-61.
7. Kujath P, Spannagel U, Habscheid W. Incidence and prophylaxis of deep venous thrombosis in outpatients with injury of the lower limb. Haemostasis. 1993;23:S20-6.
8. Kwaliteitsinstituut voor de Gezondheidszorg CBO. Richtlijn diagnostiek, preventie en behandeling van veneuze trombo-embolie en secundaire preventie arteriële trombose. 2009.
9. Lapidus LJ, Ponzer S, Elvin A, et al. Prolonged thromboprophylaxis with Dalteparin during immobilization after ankle fracture surgery: a randomized placebo-controlled, double-blind study. Acta Orthop. 2007;78:528-35.
10. Lapidus LJ, Rosfors S, Ponzer S, et al. Prolonged thromboprophylaxis with dalteparin after surgical treatment of achilles tendon rupture: a randomized, placebo-controlled study. J Orthop Trauma. 2007;21:52-7.
11. Lassen MR, Borris LC, Nakov RL. Use of the low-molecular-weight heparin reviparin to prevent deep-vein thrombosis after leg injury requiring immobilization. N Engl J Med. 2002;347:726-30.
12. Marlovits S, Striessnig G, Schuster R, et al. Extended-duration thromboprophylaxis with enoxaparin after arthroscopic surgery of the anterior cruciate ligament: a prospective, randomized, placebo-controlled study. Arthroscopy. 2007;23:696-702.
13. Michot M, Conen D, Holtz D, et al. Prevention of deep-vein thrombosis in ambulatory arthroscopic knee surgery: A randomized trial of prophylaxis with low--molecular weight heparin. Arthroscopy. 2002;18:257-63.
14. Wirth T, Schneider B, Misselwitz F, et al. Prevention of venous thromboembolism after knee arthroscopy with low-molecular weight heparin (reviparin): Results of a randomized controlled trial. Arthroscopy. 2001;17:393-9.
15. Ashrani AA, Heit JA. Incidence and cost burden of post-thrombotic syndrome. J Thromb Thrombolysis. 2009;28:465-76.
16. Jaff MR, McMurtry MS, Archer SL, et al. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation. 2011;123:1788-830.
17. Naess IA, Christiansen SC, Romundstad P, Cannegieter SC, Rosendaal FR, Hammerstrom J. Incidence and mortality of venous thrombosis: a population-based study. J Thromb Haemost. 2007;5:692-9.
18. Oger E. Incidence of venous thromboembolism: a community-based study in Western France. EPI-GETBP Study Group. Groupe d’Etude de la Thrombose de Bretagne Occidentale. Thromb Haemost. 2000;83:657-60.
19. Spencer FA, Emery C, Joffe SW, et al. Incidence rates, clinical profile, and outcomes of patients with venous thromboembolism. The Worcester VTE study. J Thromb Thrombolysis. 2009;28:401-9.
20. Anderson FA, Jr., Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003;107:I9-16.
21. Rosendaal FR. Venous thrombosis: a multicausal disease. Lancet. 1999;353:1167-73.
22. Ettema HB, Mulder MC, Nurmohamed MT, Buller HR, Verheyen CC. Dutch orthopedic thromboprophylaxis: a 5-year follow-up survey. Acta Orthop. 2009;80:109-12.
23. Schonenberg D, van MM, Nelissen RG, van der Horst-Bruinsma IE, Poll RG, Nurmohamed MT. [Thrombosis prevention in orthopaedic surgery: clinical practice in the Netherlands in 2002]. Ned Tijdschr Geneeskd. 2003;147:1856-60.
24. Truijers M, Kranendonk SE, Nurmohamed MT. [Thromboprophylaxis in general surgical practices in the year 2004: perioperative use during hospitalisation, during out-patient care and following plaster cast immobilisation]. Ned Tijdschr Geneeskd. 2005;149:2511-6.
25. Hing CB, Smith TO, Hooper L, Song F, Donell ST. A review of how to conduct a surgical survey using a questionnaire. Knee. 2011;18:209-13.
26. McColl E, Jacoby A, Thomas L, et al. Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients. Health Technol Assess. 2001;5:1-256.
27. Sprague S, Quigley L, Bhandari M. Survey design in orthopaedic surgery: getting surgeons to respond. J Bone Joint Surg Am. 2009;91 Suppl 3:27-34.
28. Ettema HB, Kollen BJ, Verheyen CC, Buller HR. Prevention of venous thromboembolism in patients with immobilization of the lower extremities: a meta-analysis of randomized controlled trials. J Thromb Haemost. 2008;6:1093-8.
29. Hoppener MR, Ettema HB, Henny CP, Verheyen CC, Buller HR. Low incidence of deep vein thrombosis after knee arthroscopy without thromboprophylaxis: a prospective cohort study of 335 patients. Acta Orthop. 2006;77:767-71.
30. Ramos J, Perrotta C, Badariotti G, Berenstein G. Interventions for preventing venous thromboembolism in adults undergoing knee arthroscopy. Cochrane Database Syst Rev. 2008;CD005259.
31. Struijk-Mulder MC, Ettema HB, Verheyen CC, Buller HR. Deep vein thrombosis after arthroscopic anterior cruciate ligament reconstruction: a prospective cohort study of 100 patients. Arthroscopy. 2013;29:1211-6.
32. Testroote M, Stigter W, de Visser DC, Janzing H. Low molecular weight heparin for prevention of venous thromboembolism in patients with lower-leg immobilization. Cochrane Database Syst Rev. 2008;CD006681.
33. Iqbal HJ, Dahab R, Barnes S. UK national survey of venous thromboembolism prophylaxis in ankle fracture patients treated with plaster casts. Foot Ankle Surg. 2012;18:157-9.
34. Ageno W, Dentali F, Imberti D. A survey of thrombosis prophylaxis use in patients undergoing arthroscopic surgery. J Thromb Haemost. 2004;2:1901-2.
35. Groves RM, Peytcheva E. The impact of nonresponse rates on nonresponse bias – A meta-analysis. Public Opinion Quarterly. 2008;72:167-89.
36. Zelnio RN. Data collection techniques: mail questionnaires. Am J Hosp Pharm. 1980;37:1113-9.