

INTRODUCTION
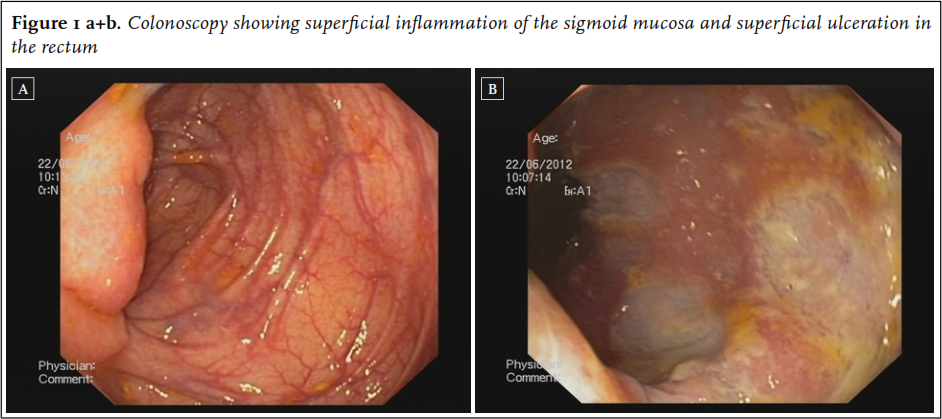
The incidence of inflammatory bowel disease (IBD) is increasing and with the ageing of the population, elderly-onset IBD will be seen more frequently. 1 Approximately 15% of IBD cases manifest in individuals over 65 years of age 1, with a similar distribution between Crohn’s disease and ulcerative colitis. IBD in elderly patients accounts for roughly 25% of all IBD-related hospitalisations. 2 Recognition of elderly-onset IBD remains poor as the differential diagnosis in older patients with a changed defecation pattern or rectal blood loss is extensive and IBD is not the most obvious cause. Furthermore, most evidence regarding IBD’s presentation, treatment and prognosis is obtained from studies excluding elderly patients or those with comorbidity. With the ageing of the population and the subsequent increasing burden of IBD in the elderly, more knowledge about this population is necessary to assure recognition, prevent treatment delays or inappropriate surgical procedures and optimise medical treatment. In this case series, three very elderly patients (> 80 years) are presented who demonstrate the difficulties in diagnosing and treating IBD in this patient population; in addition an overview of IBD in the elderly is provided. Patient A, an 84-year-old female, was hospitalised due to weight loss and diarrhoea five times a day. The diarrhoea had been present for many years and had thus far been attributed to the use of levothyroxine. Although the diarrhoea restricted her social life, no further analysis had been performed by the general practitioner. In recent months, the frequency of the diarrhoea had increased, resulting in hospitalisation. On admission, physical examination revealed multiple perianal fistulae. Colonoscopy identified superficial inflammation of the sigmoid mucosa ( figure 1) as well as several fistulae and superficial ulceration in the rectum. Tissue biopsies revealed an inflammatory infiltrate with granulocytes and impairment of the crypt epithelium, focal ulceration of the colon mucosa and non-specific chronic active inflammation. Spirochetes and Ziehl-Neelsen staining and Elispot were negative as was the tuberculin skin test. Magnetic resonance imaging (MRI) confirmed the ulceration of the rectum extending into the internal anal sphincter as well as a suprasphincteric fistula and an intersphincteric fistula. Both macroscopic and microscopic findings were compatible with Crohn’s disease. Because she was not experiencing any pain, surgical treatment was not indicated. Treatment with metronidazole, ciprofloxacin and prednisolone was started as well as azathioprine therapy. At discharge, the prednisolone was tapered by 5 mg per week. However, due to persistent production of the fistulae and perianal pain, treatment with infliximab was started during follow-up. After three infusions, the symptoms resolved and the prednisolone was stopped. Maintenance therapy with azathioprine and infliximab was continued and her diarrhoea resolved.
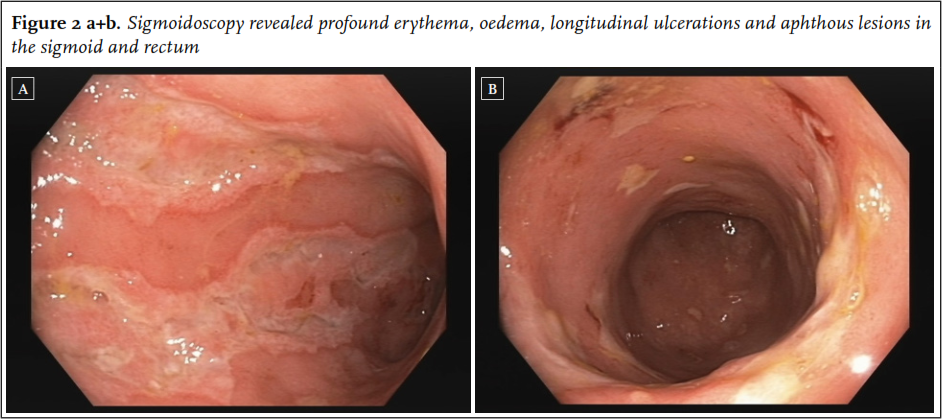
Patient B, an 87-year-old female, visited the geriatric clinical centre because of constipation. For over a year, she had had slow bowel movements without any further symptoms. Treatment with psyllium was successful, however when stopping the medication her symptoms returned. As physical examination and biochemical testing did not reveal any abnormalities, she was given further advice regarding the constipation and treatment with psyllium was restarted. One year later, she developed diarrhoea up to five times a day with faecal incontinence and infrequent rectal bleeding. She had lost 10 kg in the course of a few months. Infectious colitis was ruled out with negative stool culture. Laboratory testing revealed an elevated erythrocyte sedimentation rate (> 95 mm/hour) and a computed tomography of the abdomen displayed increased signal intensity of the sigmoid compatible with colitis. Sigmoidoscopy was performed and revealed profound erythema, oedema, longitudinal ulcerations and aphthous lesions in the sigmoid and rectum while the distal rectum did not show any abnormalities ( figure 2). Histopathology revealed alternating active inflammation and normal mucosa and many granulocytes in the lamina propria. Microscopic findings were non-specific, but considering the clinical presentation and endoscopic findings, therapy for IBD was initiated. Infection with Mycobacterium tuberculosis was excluded. As treatment with budesonide achieved an insufficient effect, prednisone was started at 30 mg daily in a tapering schedule together with psyllium. Initially, remission was induced successfully; however, her symptoms returned at a dose of prednisone 5 mg daily. Therefore, budesonide and azathioprine were started which achieved a good response.
Patient C, an 84-year-old female, was admitted to the hospital with progressively painful abdominal cramps during the last years. Her medical history included diabetes mellitus type II and in 2011 ulcerative proctitis with complaints of rectal bleeding and difficulty with defecation. For two years she was successfully treated with 5-aminosalicylate (5-ASA) enemas. At current admission, this treatment was no longer sufficient. Her defecation pattern had changed again, alternating between constipation and diarrhoea with occasionally red blood loss per anum. She complained about uncontrollable flatulence and sometimes faecal incontinence. In six months, she had lost 5 kg in weight. Colonoscopy and biopsy findings were suggestive of severe Crohn’s disease extending from the terminal ileum to the rectum. Treatment with dexamethasone intravenously was started, which was complicated by moderate hyperglycaemia. Her abdominal symptoms improved significantly and therapy was switched to oral prednisolone 30 mg tablets in a tapering schedule. Infection with M. tuberculosis was excluded. Subsequently, she was treated with azathioprine as maintenance therapy, which achieved a good clinical response.
BACKGROUND AND SYMPTOMS
The present case series describes three very elderly patients (> 80 years) with late-onset IBD. We were specifically interested in late-onset IBD in the very elderly, not to be confused with long-standing IBD in elderly patients. However, except for a few case reports, literature regarding this very old population is scarce. Therefore, we considered best available evidence, studies including IBD patients with onset of disease after the age of 60 years. Crohn’s disease and ulcerative colitis are inflammatory bowel diseases, characterised by progressive, chronic inflammation of the gastrointestinal tract. Their aetiology remains to be unravelled. However, genetic, immunological and environmental factors all appear to influence the development of IBD. 3-6 IBD may occur at any age but a bimodal course has been reported. Although there is a preference for adolescents, approximately 10-30% of all new IBD patients are over 60 years of age. Of these 65% are in their 60s, 25% in their 70s and only 10% in their 80s. 7,8 The estimated incidence of IBD in patients over 60 years in Europe is 8-10/100,000. 9-11
Crohn’s disease and ulcerative colitis are separate entities but distinction can be difficult. In ulcerative colitis, inflammation is limited to the colon and generally has a diffuse and superficial character. Crohn’s disease, on the other hand, is characterised by a discontinuous transmural inflammation and may involve the entire digestive tract including the mouth and perianal area. In younger patients, the distal ileum and colon are frequently involved. However, in older patients, the primary location of Crohn’s disease is the colon, making the distinction from ulcerative colitis less obvious. 12
Clinical presentation in the elderly can be non-specific. Elderly patients may have had symptoms for many years – as demonstrated by patient A – before the diagnosis is established. 13 The average time to establish the diagnosis is six years in the elderly compared with two years in younger patients. 13 Hallmarks of Crohn’s disease are prolonged diarrhoea with crampy abdominal pain without gross bleeding and systemic symptoms as weight loss, fatigue and fever. In ulcerative colitis, patients often present with bloody diarrhoea and frequent bowel movements. Elderly patients with IBD appear to have a less complicated and milder disease course compared with younger patients, 14 but will more often experience weight loss, anaemia and abdominal pain. 13,15 The disease course is different from young-onset IBD patients as disease extension rarely occurs in the elderly. 16 However, in patient C disease extension was seen. In elderly patients, constipation can also be the presenting symptom of IBD. 17 Although patient B had suffered from constipation for a year prior to IBD diagnosis, she did not experience any other symptoms at that time, making it less likely that the constipation was related to the Crohn’s disease.
Differential diagnostic considerations
As the clinical presentation can be rather non-specific, particularly in the elderly, there is a long list of potential differential diagnoses. Other more prevalent disorders will often be considered initially, resulting in misdiagnosis and delays in initiating the appropriate treatment. 18
In every elderly patient presenting with new abdominal symptoms, the differential diagnosis should include colorectal malignancy. Furthermore, colonic diverticulitis and segmental colitis associated with diverticular disease are causes of an altered defecation pattern or rectal blood loss in the elderly and may be easily confused with IBD. A relatively common cause of diarrhoea in the elderly is microscopic colitis, but it is rarely confused with IBD because of the lack of visible mucosal inflammation. Many drugs can also elicit abdominal symptoms or result in complications inducing those complaints, such as colonic ulcers induced by antibiotics and ulcers and strictures caused by non-steroidal anti-inflammatory drugs. In the initial phases of disease, IBD may also be confused with infectious diarrhoea. In patients with a history of radiation to the abdomen, one must be aware of the possibility of radiation enteropathy. Another differential diagnostic consideration not to be missed is ischaemic colitis. These patients often present with acute abdominal pain and subsequently bloody stools. In patients with generalised peripheral arterial occlusive disease or mesenteric arterial thrombosis or embolism, inadequate blood flow causes segmental inflammation and injury of the colonic mucosa and in case of more profound ischaemia also transmural colonic damage. There is considerable overlap in the signs and symptoms of ischaemic colitis and Crohn’s disease. Both often present with rectal preservation and a segmental distribution of disease, contrary to ulcerative colitis. Distinction is based on the combination of clinical, endoscopic and histological findings. Furthermore in ischaemic colitis repeat colonoscopy may show rapid resolution of lesions. Unfortunately, we did not repeat the colonoscopy after starting therapy to confirm the clinical response, which ideally should have been performed. In patient B, histological findings were non-specific and it could be discussed whether the diagnosis IBD is definitive. However, clinically she showed a good response to therapy. As endoscopy can be a strenuous investigation in elderly patients, it cannot always be repeated.
Because of the extended differential diagnosis of abdominal symptoms in the elderly, imaging studies and colonoscopy should be readily performed. If endoscopy and histology reveal findings compatible with inflammation and ulceration, IBD must be considered, even in patients over 80 years of age, as our cases illustrate.
Therapy
The choice of treatment will depend on multiple factors, including the severity, location and extension of disease, disease behaviour, extra-intestinal manifestations, comorbidity, use of other medications and patient compliance. Irrespective of treatment choice, maintaining adequate nutritional status is important. Malnutrition is relatively common in the older population, which can also affect treatment tolerance and increases the risk of infections. Furthermore, elderly-onset IBD has a less aggressive disease course, 14 and this has to be taken into account when making therapeutic decisions. On the other hand, over half of patients aged 65 years or more have at least three comorbidities and a recent study illustrated that elderly patients with Crohn’s disease take a mean of 6.6 types of concurrent medication, 19 increasing the risk of drug interactions and adverse events.
5-aminosalicylates
First choice for treatment of mild to moderate ulcerative colitis is topical or oral 5-ASA. The use of 5-ASA in Crohn’s disease is controversial due to inconsistent results regarding its efficacy. 20 Efficacy seems to be comparable in both young and elderly patients. 21 There are conflicting results regarding the renal impact of 5-ASA. Cases of 5-ASA nephrotoxicity and interstitial nephritis have been rarely reported, 22 but most did not demonstrate a relationship with the 5-ASA dose or duration of usage. 23,24 Evidence regarding the use of 5-ASA in elderly patients with impaired renal function is lacking. It is recommended to exercise caution in patients with known renal dysfunction and to evaluate renal function prior to initiation of 5-ASA and periodically thereafter.
Corticosteroids
Patients with mild to moderate ileal or ileocaecal disease, severe ulcerative colitis or those not responding to 5-ASA can be treated with oral corticosteroids. Induction therapy with budesonide is usually recommended for mild to moderate ileal or ileocaecal disease, as this causes less systemic side effects than other glucocorticoids. In patients who do not respond to oral therapy, temporary intravenous administration of corticosteroids may be necessary. Corticosteroids should not to be used as maintenance therapy because of decreasing efficacy in long-term use and side effects such as osteoporosis, risk for serious infections, 25 hyperglycaemia, cataract and neuropsychiatric disorders. 26 When starting glucocorticoids, appropriate osteoporosis prophylaxis according to guidelines should be started.
Immunomodulators and biological therapy
In patients who do not respond to oral glucocorticoids, the addition of immunomodulatory drugs (azathioprine and 6-mercaptopurine, 6-MP) or monoclonal anti-TNF antibodies can be considered. No differences in efficacy, metabolism and toxicity of immunomodulators have been found between older and younger patients. 27,28 They are generally well tolerated with a relatively low incidence of adverse effects. Adverse events include idiosyncratic reactions (fever, rash, pancreatitis and hepatitis) and bone marrow suppression. 29 Hence it is important to check the complete blood count and liver chemistry regularly. Possible drug interactions should be checked before starting therapy.
Biologicals are infrequently used in elderly IBD patients because of a lack of data regarding their use in this population. However, some data are available on the use of biologicals in patients with rheumatoid arthritis. Results regarding the occurrence of adverse events in the elderly are conflicting, with some suggesting a higher risk of serious adverse events such as infections while others did not. 30-32 We believe biologicals should be considered in elderly patients when other therapeutic strategies fail and contraindications for their use – such as congestive heart failure, significant hepatic disease and concomitant infections – have been excluded. In patient A, glucocorticoids and azathioprine therapy achieved insufficient results and then infliximab was started successfully.
Almost all agents used for IBD (corticosteroids, immunomodulators and biologicals) will compromise the patient’s immune response to infectious agents. The odds for opportunistic infections is increased threefold (OR 2.9; 95% CI 1.5-5.3) when corticosteroids, azathioprine, 6-mercaptopurine or infliximab are used as monotherapy. 31 However, the risk of infection increases considerably when two or more drugs are used concomitantly (OR 14.5; 95% CI 4.9-43). 31 As elderly patients have a higher incidence of latent tuberculosis infection and higher mortality rates due to reactivation of M. tuberculosis when immuno suppressive treatment is started, 33 it is of particular importance to exclude latent tuberculosis infection prior to starting treatment. Furthermore, intestinal tuberculosis may mimic IBD’s findings at colonoscopy and therefore should be excluded.
Surgery
When medical options do not achieve the desired results or in case of toxic megacolon, obstruction, fistula formation or incessant bleeding, surgery may be necessary. Recent reports suggest that indications for surgery in the elderly with ulcerative colitis should not differ from indications for surgery in younger patients. 34 However, the need for urgent surgery in the elderly was also a predictor of poor survival. 35 Furthermore, despite a significant decrease in the frequency of surgery-associated adverse outcomes in the elderly with ulcerative colitis, adverse events still occur in 27% of patients. 36 In addition to increased rates of postoperative complications, an increased length of hospital stay and increased operating room time have also been reported in the elderly with IBD. 37 Factors associated with poor outcome included male gender, low albumin levels and advanced age. 36
With regards to Crohn’s disease, elderly patients – who more often have colonic disease – undergo fewer surgical procedures compared with younger patients. 38 Surgery for complications of Crohn’s disease in the elderly are technically not different.
After colectomy, restorative coloproctectomy with ileal J-pouch anal anastomosis (IPAA) can be successful provided the patient retains good anal sphincter function, has no history of faecal incontinence preoperatively and is autonomous. In the very old, one should carefully assess all these items when considering IPAA because problems are supposed to be more likely to develop in this age group. Recent studies in patients with IPAA showed no differences concerning complication rate and quality of life and function in the elderly compared with the younger population. 39,40 Patient satisfaction is high after IPAA: over 89% of patients older than 65 years report that they would undergo the same surgery again and more than 93% would recommend it to others. 41 It is not known if these data also pertain to the oldest old or can be extrapolated to older patients with comorbidities.
If IPAA is not possible, a protocolectomy or subtotal colectomy and end ileostomy can be performed. 42,43 Ileorectal anastomosis, mostly abandoned in young ulcerative colitis patients, still has indications in the elderly with lower life expectancy when functional outcome is most important. 44 Although ostomies are not uncommon and generally well-tolerated in the elderly, it is important to note these patients are more likely to suffer from dehydration due to stoma output when compared with younger patients. 39
In conclusion, diarrhoea, abdominal symptoms and an altered defecation pattern in the elderly may have many causes. Elderly-onset IBD does not occur frequently and clinical features are non-specific, thus establishing the correct diagnosis is a challenge. However, not considering this diagnosis leads to delays in initiating the appropriate treatment, as well as potential preventable complications and persisting morbidity. Colonoscopy should be readily performed in the elderly in order to differentiate within the broad list of potential disorders compatible with abdominal symptoms. If endoscopy and histology reveal findings compatible with inflammation and ulceration, IBD must be considered, even in the very old. Although the choice of medical therapy is not essentially different from younger patients with IBD, elderly patients should be carefully monitored when medical therapy is started in order to avoid serious complications.
DISCLOSURES
No conflict of interest; no financial disclosures.
REFERENCES