

KEYWORDS
Acute care, emergency department, healthcare organisation, internal medicine
INTRODUCTION
The demand on the health care systems and the emergency department in particular, is increasing.1,2 This leads to crowding and queuing, negatively influencing the quality of care.3 It manifests as long lengths of stay in EDs, adverse clinical outcomes, and poor patient experience.3-5 Over the last years, it has been stated that this could impede the accessibility of the acute care, locally and internationally.4,6,7
For several years, there has been ongoing discussion about the reorganisation of the acute care system in the Netherlands, creating disagreement between hospital organisations and health insurers.8 Many reports have been published on this topic, aiming to gain insight into the use and accessibility of Dutch emergency care.1,9-13 Factors such as patient flow, healthcare costs, and predicted future demographic changes are subjects of these reports and are used in decision making processes by policymakers. Key issues for shaping the acute landscape with intended preservation of quality are, for example, centralisation of complex care and the presence of a doctor in the ED with at least one year of working experience.14 However, organisation of emergency care for acute medical patients and of EDs especially, differs between hospitals, mainly in number of physicians, the presence of (supervising) internists in the ED, working agreements between internists and emergency physicians (EP), the presence of an Acute Medical Unit (AMU,) and collaboration with the general practitioner out-of-hours services, known as General Practitioner Cooperatives (GPC).15-17 Insight into similarities or differences of these characteristics and eventually their influence on patient outcomes would help to make well-founded choices in reshaping the acute care chain for acute medical patients.
It is known that the organisation of the acute care chain may influence the quality of delivered care and performance of the ED.18 Internal factors such as staffing, number of patients, and number of treatment bays, and external factors such as demographics and underlying financial resources, have already been identified as having an influence on ED performance.19 Moreover, these factors will also complicate evaluation and comparison of ED performance. In addition, many acute medical patients, especially the elderly, have multimorbidity or polypharmacy and present themselves to the ED with undifferentiated problems which makes it challenging to differentiate between the influence of internal factors of the ED and patient-related factors on outcomes. Given the complexity of this patient group increasingly presenting in the acute care chain, the Netherlands Association of Internal Medicine has stated in their strategic vision that internists should play a coordinating role in the acute care of patients with multimorbidity and polypharmacy.20 Yet, an important subject in order to improve the quality of acute care, is identifying potential actors on performance and outcomes of the local hospital organisation, such as the physical presence of internists in the ED. Therefore, it is important to create a sufficient overview of ED care, focusing on (acute) internal medicine, in the Netherlands.
When investigating the influence of organisation on patient outcomes, it is essential to first evaluate the organisation, including staffing and working arrangements between EPs and internists. We believe that this detailed overview is necessary for creating a foundation for scientific research nationally and also internationally. In addition, this will also make comparisons between care for acute medical patients in the Netherlands and internationally more insightful. Finally, we will reflect on the public discussion regarding acute care and formulate critical notes for future organisational models based on this overview, aiming to improve the quality of care for acute medical patients.
METHODS
Design
We performed a nationwide observational study, identifying the organisational structure of EDs in the Netherlands. All hospitals with an ED in the Netherlands were identified in January 2018. At the start of the study, we identified 91 EDs within 76 hospital organisations and 89 EDs at the end of the study (February 1st, 2019) due to the closure of two hospitals. An acute internist, if present, or a consultant internal medicine physician with an affinity for acute care, was contacted by e-mail to participate in the study and an online questionnaire was distributed (using Qualtrics XM, U.S.A.). In addition, administrative hospital data of patient numbers between January 1st, 2013 and December 31st, 2017 in a predefined format (supplementary data) were collected. The total number of patients visiting the ED, the number of patients older than 65 years, the number of patients visiting the ED for internal medicine, and admissions for internal medicine were requested. The results of the questionnaire including patient numbers, were directly transferred to the study database in SPSS Statistics 25.0 for Windows. The study period of the online questionnaire was between January 2018 and February 2019. Reminders were sent every 2-3 months by e-mail, to all identified physicians at the beginning of the study. Three researchers (MK, HH, PN) contacted the invited physicians who did not respond to the questionnaire by telephone. This was done in December 2018 and January 2019, in an ultimate effort to collect as much data as possible. No effort was made to retrieve missing data. A full overview of definitions used in the questionnaire is provided in appendix 1. Words that are associated with a definition in the appendix are marked with an asterisk (*). Our goal was to obtain participation of at least 66% of all EDs, divided over the country. Participation was voluntary and the study protocol was approved by the Medical Ethics Committee of Máxima MC (study number N17.122).
Setting
In the Netherlands, 2.4 million ED visits were registered in 2016 and 840,000 (35%) patients were admitted (total country population of 17 million).1 To gain access to hospital care in the Netherlands, including EDs, patients are required to have a referral from a GP or directly transferred by an ambulance.15 Self-referral is possible, however a deductible reduction has been introduced to discourage self-referrals.21 During out-of-hours, GPs in the region cooperate to provide urgent primary care on a rotation basis, taking care of each other’s patients in GPCs. This ensures a gatekeeping function of the GP, around the clock. GPCs can collaborate with the local ED, varying between no collaboration to an integrated GPC in the ED.13 In general, residents of different medical specialties staff the ED in collaboration with residents in emergency medicine, supervised by medical specialists and EPs, depending on the local organisation and working agreements. All residents are qualified doctors who are either in training to become specialists or non-trainees who are working in the hospitals to gain experience with the aim of entering a specialist training programme. Only since 2009, has emergency medicine been recognised as a specialty, however in 2000, the first hospitals started to train EPs aiming to introduce EPs into the ED.22 Yet, until now, EPs are not fully integrated into every ED. Acute internal medicine has been recognised as subspecialty within internal medicine since 2010.23 Internists are present in each hospital, whereas acute internists are not.
Statistical analysis
Descriptive statistics were executed using IBM SPSS Statistics 25.0 for Windows. Missing data were categorised as ‘missing’.
RESULTS
In total, we gathered data from 76 out of 89 EDs (84%) within 67 hospital organisations of different types (table 1). The EDs were evenly spread over the country as is shown in figure 1. Thirteen EDs (16%) did not respond to the online questionnaire and we were unable to reach an internist at these locations by telephone. Of these, four EDs were located in a teaching hospital* and nine EDs in a general hospital*.
ED characteristics
From a total of 76 EDs, 72 were operational full time (24/7). The remaining four EDs were closed during the night or reported another (undefined) schedule, as is shown in table 1. At 47 EDs (62%), a separate cardiac ED was present; 17 EDs did not have a separate cardiac ED and 12 EDs did not mention their organisation for acute cardiac patients.
The type of collaboration between EDs and the GPC is shown in table 1. A GPC serial* to the ED or integrated* within the ED were the most frequently reported types of collaboration. The presence of EPs or internists in the ED was not associated with the type of collaboration with the GPC (Fisher’s Exact Test: 11.08; p = 0.47, respectively 19.27, p = 0.13).
An AMU* was present at 39 locations (51%), not present at 29 locations (38%), and 8 locations (11%) did not report if an AMU was present. At locations equipped with an AMU, an acute internist was present* in 72% of these locations, while at locations without an AMU, an acute internist was only present at 55% of these locations. 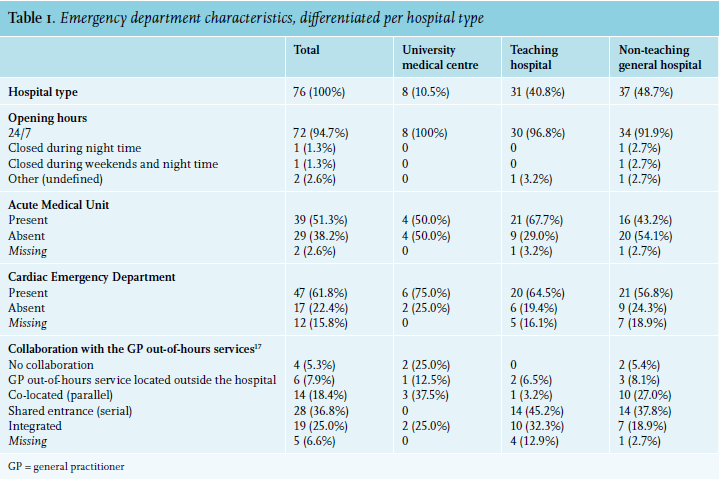
Between 2013 and 2017, 41 EDs reported numbers of patients visiting the ED. Of these, eight EDs did not provide numbers beyond 2016. Patient numbers were collected from eight EDs located in university medical centres*, 18 in teaching hospitals*, and 15 in general hospitals*. Since 2013, there has been a decrease in the total number of patients visiting the ED. In 2013, on average 22,359 patients (range: 7,857-42,488) visited the ED compared to 20,818 patients (range: 7,775-42,488) in 2017. This is a decrease of 6.9%. The number of patients ≥ 65 years has increased over the years by 7.3%. In 2013, 6,699 patients (range 3,685-10,245) older than 65 years visited the ED and 7,230 (range: 3,404-13,389) in 2017. EDs located in university medical centres and teaching hospitals are similar in the total number of patients visiting the ED (± 23,500 on average in 2017), while EDs in general hospitals had fewer ED visits (± 16,500 on average in 2017).
The number of patients presenting for internal medicine increased slightly from 2013 to 2016, but showed a decrease in 2017. In 2013, 3,824 patients (range: 1,227-10,403) presented to the ED for internal medicine, compared to 4,343 patients (range: 1,418-29,426) in 2016 and 3,855 patients (range: 1,505-20,832) in 2017. This decrease is only visible in EDs in general and teaching hospitals, while university medical centres showed an increase of patients presenting to the ED for internal medicine. In addition, there is a slight overall decrease in the number of patients ≥ 65 years presenting for internal medicine, but only between 2016 and 2017. The percentage of patients ≥ 65 years presenting for internal medicine, as part of the total number of patients ≥ 65 years visiting the ED, has also decreased over the last years (figure 2).
ED Staffing
EPs were present in 60 EDs (79%), of which there were EPs 24/7 in 32 EDs (46%). If EPs were not present 24/7, they were mostly absent during night hours or had another (undefined) working schedule (table 2). At 51 locations (67%), a registered acute internist is employed. Absence of a registered acute internist was most common in general hospitals*: 68% absence versus 32% in teaching hospitals* and 0% in university medical centres*. While internists are employed and present in all hospitals, their presence* in the ED differs: at 10 locations (13.2%) internists reported not being able to present in the ED for supervision because of other tasks at the same time. In 17 EDs (22.4%%), the internist is on call, without a working place near the ED, and therefore may or may not be present when a patient arrives. In 6 EDs (8%), the internist was physically present at least during office hours and evenings in the ED. In absence of an EP, the internist is more often present in the ED during office hours [11 out of 16 EDs (68.8%)], compared to EDs with 24/7 coverage of EPs [18 out of 31 EDs (58.1%)].
Internal medicine residents treat patients for internal medicine in 65 EDs (86%), as shown in table 2. In 11 EDs (14%), all located in a general hospital, there are no internal medicine residents treating patients in the ED. Patients in these hospitals are treated by emergency care residents, EPs, or internists. However, in the majority of university medical centres and teaching hospitals (92%), patients are seen by residents in training as well as residents not in training. Residents in training are present in 15 EDs in general hospitals (48%), while residents not in training are present in 26 EDs (84%). Supervision is provided by internists and/or EPs.
Roles and responsibilities
Internists reported having various roles in the ED: 68 internists (89.5%) were practitioners*, 57 consultants* (75.0%), 22 coordinators* (28.9%), and 15 managers (19.7%); 3 internists did not report their role. In addition, 6 internists (7.9%) mentioned other roles, such as supervisor and trainer. Internists working in a university medical centre seemed to be more frequently a coordinator and manager in comparison with internists in teaching or general hospitals. Furthermore, the presence of an acute internist was associated with reporting these coordinating and managing roles frequently. In hospitals where EPs were not present, internists more often reported a role as practitioner compared to hospitals where no EPs were present (100% vs. 87.1%) and consultant (93.8% vs. 64.5%).
We assessed working agreements between internists and EPs by taking inventory of who was in the lead during the initial care* of medical, haemodynamically instable patients. These arrangements were different for referred* and not referred* patients. In general, the initial care of referred patients is led by the internist (39%) or internal medicine resident (46%). Non-referred patients are most often treated by the EP (60%), if present. Secondly, we assessed supervision agreements. Patients who were referred and assessed by residents were supervised by internists at 71.1% of the EDs, by an internal medicine fellow* at 7.9% of the EDs, and by EPs at 14.5% of the EDs. Fourteen EDs (18.4%) did not report their supervision agreements. Supervision of residents treating non-referred patients is equally divided between EPs and internists. Furthermore, EPs must contact the internist to admit acute medical patients at all of the 47 responding EDs. Discharging patients directly from the ED without contacting the internist is only acceptable in cases of non-referred patients at 18 of the 36 responding EDs (50.0%).
Lastly, internists graded the collaboration with EPs in the ED with a mean of 7.4 out of 10 (range: 1 to 10). There was no difference in grading in presence or absence of an acute internist. Transparent working agreements, being approachable, and logistic support were mentioned as strengths. Internists experienced variation between EPs in the quality of delivered care, especially in complex multimorbid patients. For example, one internist’s opinion, “There’s a continuous conflict of domains and EPs have a poor knowledge of internal medicine”. In contrast, another internist reported, “We experience a perfect interprofessional collaboration and we make use of each other’s expertise”. In addition, some internists preferred to be contacted in an earlier stage by the EP for consultation.
DISCUSSION
We provide a detailed overview of the organisation of the Dutch acute care in the ED, focusing on acute internal medicine combined with the roles and presence of EPs. Our study shows that there is a decrease in the number of patients arriving at the ED, while there is an increase in patients of 65 years and older. However, in 2016, there was a slight decrease in patients of 65 years and older presenting to the ED for internal medicine. Furthermore, we identified differences in the presence of (acute) internists and EPs in the ED and a variability in working and supervision agreements. Internists reported their roles at the ED most often as practitioner and consultant. Internists experienced the collaboration with EPs as satisfactory.
We showed that patients 65 years and older are an increasing population in the ED in the Netherlands, which is also an international trend.2,24 In general, internists are trained to provide complex care to acute patients regarding aging, multimorbidity, and polypharmacy. However, we assessed that patient visits for internal medicine among patients 65 years and older decreased in 2017, which is the contrast with the overall growth of this population in the ED. This decrease remained also present when correcting for missing data. Several reasons may be suggested for this decline, such as older patients encounter problems other than acute illness, or patients are triaged to specific disciplines (i.e., pulmonology, cardiology, or even geriatrics) by EPs. However, this discussion is beyond the scope of this article.
The most notable finding of this study is the number of internists (14%) not physically present in the EDs. In addition, some internists did not identify themselves as a practitioner* (10.5%) nor a consultant* (25%). These statements are a remarkable finding, because both observations are in contrast with the current strategic vision of the Netherlands Association of Internal Medicine, which states that internists should be the central contact for acute medical patients with multimorbidity and polypharmacy.20 The literature has not shown best practices on this matter yet, although one Dutch study has shown that the presence of medical specialists, including internists, leads to improved patient flow and satisfaction.25 In addition, internists are specialised to take care of multimorbid patients with polypharmacy.20,26 Given the increased case complexity of acute patients presenting to the ED due to multimorbidity and polypharmacy, internists can play a central role in the care for these patients.27,28 In addition, most patients suffer from an acute deterioration of a chronic disease. These patients need a specialist with knowledge of the disease course prior to the ED visit, diagnostic and treatment possibilities considering comorbidities and medication use, and coordination of follow-up. As acute care needs teamwork, EPs can play an important role in the initial care of acute medical patients. It has been shown that activities in the patient care process and patient flow differ between internists and EPs, which may suggest that internists and EPs could be complementary to each other.29 However, in this study, we found signs of suboptimal interprofessional collaboration between EPs and internists in some hospitals. A qualitative study about interprofessional collaboration between internists and EPs as well as a quantitative study on outcomes, could provide useful insight in this subject and the effects on quality of care.
We showed many organisational and staffing differences between different EDs across the Netherlands, such as the presence of internists at the ED, variability in working agreements in initial care* of haemodynamically instable patients, and collaboration choices with the GPCs. These data concur with research in the field of acute medical care from, for example, the United Kingdom (UK), which also showed differences in structure and staffing (in this case AMUs) and even more interesting, that patient flow also vary per hospital.30-32 However, in contrast to the recently developed Dutch quality standards for acute care,14 it may not be achievable and desirable to pursue one uniform organisation for all EDs in the Netherlands. It has been shown that regional and local external factors are known to influence performance of the ED and differences in organisation could be beneficial, if adapted to the local characteristics.19,33 In this study, we identified these differences in organisational structure, which should be investigated further in order to evaluate impact on the quality of acute care. The yearly Society for Acute Medicine Benchmarking Audit performed in the UK is an interesting tool which can be used as an example to provide insight into the performance of acute medical care, which also take organisational differences into account.32 In addition, the identified differences in organisational structure should have a place in the interpretation of scientific research concerning acute care and used as context, assuring benefit of potential changes in treatment or organisation in the local situation.34 Finally, we would recommend to use this overview to interpret and evaluate international differences in acute care.
Recommendations and future directions
We emphasise further research on the influence of the organisation of acute care on the quality of care, aiming to make well-founded choices in the future organisation of acute medical care, at least in the Netherlands. In order to evaluate these organisational factors, we recommend a national registry for acute medical care including patient outcomes, ED characteristics, and regional organisational characteristics of the acute care chain. In addition, we believe that relevant Patient Reported Outcomes for acute care should be evaluated regularly and incorporated in this registry.35 Structural measurements of performance in acute medical care could help to make sensible and evidence-based organisational choices. Secondly, we recommend that internists increase their presence in the ED and availability for ED care, and aim to be the central contact for acute medical patients with multimorbidity and polypharmacy in accordance with the current strategic vision of the Netherlands Association of Internal Medicine.20 Internists have the knowledge and expertise to treat this specific group, however, we demonstrated that in 2018, their presence was suboptimal in EDs in quite a few hospitals. As case complexity increases, patients deserve specialised care provided by a doctor who is capable of overviewing all problems and able to arrange and provide proper follow-up. Therefore, the presence of internists in the ED and their influence on the quality of care should be investigated further. This observational study could be used as a reference.
Limitations
Unfortunately, we were unable to receive responses from all EDs in the Netherlands. However, we achieved a response rate of 84% by sending reminders and even trying to reach internists by telephone. As the responding EDs were fairly divided over the country and representing university medical centres, teaching hospitals, and general hospitals, we postulate that the selection bias is minimal. Only 41 EDs reported on patient numbers and of these EDs, patient numbers beyond 2016 were not provided by eight EDs. Therefore, interpretation of these data demands some caution. In addition, due to the use of multiple-choice questions, it was difficult to interpret answers in the local context or identify motives in organisational choices.
CONCLUSION
To our knowledge, this is the first study that provides a detailed overview of ED organisation in the Netherlands regarding internal medicine patients. Our study shows that organisation of ED care for internal medicine patients differs in terms of staffing, presence of EPs and internists, and working agreements between EPs and internists. Some of these differences, such as the presence of internal medicine residents in the ED, seem to depend on the type of hospital. As it is known that regional and local external factors influence performance of the ED, local and regional differences in the organisation of acute medical care should be taken into account when developing nationwide quality standards for acute care and future research should be used to create a more evidence-based policy. Given the assumed increased case complexity of medical patients, we believe that internists should be the central contact for these patients and therefore should be present frequently at the ED.
ACKNOWLEDGEMENTS
Grant support
This study was funded by the science fund of the Netherlands Association of Internal Medicine. The authors declare that they have no competing interests. We thank all the internists who took part in the study and special thanks to the members of the ORCA (Onderzoeks Consortium Acute Geneeskunde) Acute Medicine Research Consortium for their cooperation.
Members of the ORCA consortium are: Nanayakkara PWB, Amsterdam University Medical Center, location Vu University Medical Center, the Netherlands; Haak HR, Máxima MC, the Netherlands; Alsma J, Erasmus University Medical Center, the Netherlands; Kremers MNT, Maastricht University and CAPHRI School for Public Health and Primary Care, Aging and Long Term care Maastricht, the Netherlands; Uffen JW, University Medical Center Utrecht, the Netherlands; Fogteloo AJ, Leiden University Medical Center, the Netherlands; Groeneveld GH, Leiden University Medical Center, the Netherlands; Bauer MP, Leiden University Medical Center, the Netherlands; Carels RA, Ikazia Hospital, the Netherlands; Dees A, Ikazia Hospital, the Netherlands; Schuit SCE, Erasmus University Medical Center, the Netherlands; Brouwer R, Medisch Spectrum Twente, the Netherlands; Brink H, Medisch Spectrum Twente, the Netherlands; Holleman F, Amsterdam University Medical Center, location AMC, the Netherlands; van Nieuwkoop C, Haga Teaching Hospital, the Netherlands; Hoogerwerf JJ, Radboud University Medical Center, the Netherlands; Kaasjager KHAH, University Medical Center Utrecht, the Netherlands; Vrijsen BEL, University Medical Center Utrecht, the Netherlands; Schouten WEM, OLVG location East, the Netherlands; Ter Maaten JC, University Medical Center Groningen, the Netherlands; Ligtenberg JJM, University Medical Center Groningen, the Netherlands; Stassen PM, Maastricht University Medical Center, the Netherlands; van Noord C, Maasstad Hospital, the Netherlands; van Leeuwen-Nguyen HTT, Maasstad Hospital, the Netherlands; Govers A, Sint Franciscus Gasthuis & Vlietland, the Netherlands; Bosch FH, Rijnstate Hospital, the Netherlands; Buunk G, Amphia Hospital, the Netherlands; van Herpt TTW, Amphia Hospital, the Netherlands; de Regt MJA, OLVG, the Netherlands.
REFERENCES