

KEYWORDS
PoCUS, point-of-care ultrasound, ultrasound for internists, ultrasound curriculum, EPA
INTRODUCTION
Point-of-care Ultrasound (PoCUS) is defined as ‘diagnostic or procedural guidance ultrasound that is performed by a clinician during a patient encounter to help guide the evaluation and management of the patient’.1 This technique is useful in the primary assessment of acutely ill internal medicine patients and enhances diagnostics and resuscitation as it adds clinical data which cannot be obtained by physical examination.2 This ‘stethoscope of the 21th century’ is quickly developing, is easily accessible with improved portability, produces images of increasing quality, and is more affordable; however, the diagnostic performance is largely operator-dependent and it is not known how many PoCUS exams a sonographer needs to perform to obtain reliable results.3 Medical treatment decisions can be guided by ultrasound results; therefore, it is essential that these results are trustworthy. In the Netherlands, ultrasound was first advocated in 2012 as a useful complementary skill for internists in the management of acutely medically ill patients.4 Today, mandatory PoCUS training is included in the education of internists as stated by the Dutch internal medicine federation (Nederlands Internisten Vereniging, NIV) and a national training program that is currently under development.5 However, there are not enough ultrasound experts to provide education to all internal medicine residents, and it is questionable if every internist should be fully competent for every PoCUS indication. Regardless, proper training is critical for both current and future ultrasound applications within internal medicine.
Existing ultrasound curricula for emergency medicine physicians can be used as guidelines to develop an ultrasound curriculum for internists. For example, the American College of Emergency Physicians (ACEP) has published a revised policy statement on ultrasound guidelines in which they define 12 core PoCUS applications with proven benefit (table 1).6
The International Federation for Emergency Medicine (IFEM) has published a similar PoCUS curriculum guideline which describes the content of an ultrasound program and the method for training and practice.1 In Italy, the ultrasound training program for internal medicine residents consists of a two-step level of competence concerning a variety of clinical presentations and diagnosis divided into five modules.7 Other European countries have ultrasound training programs as well but these programs do not meet the needs of an ultrasound curriculum as defined by the Dutch Internal Medicine Federation.8,9 The content of a PoCUS curriculum is determined by regional and national differences as it should be relevant to local and national practice. Therefore, an ultrasound curriculum relevant for internists in the Netherlands is needed. This includes selecting the most relevant core applications for internists and describing how competency in ultrasound is obtained. Achieving competency consists of initial introduction and basic training in ultrasound, gaining experience, assessing competency, and staying competent. In this article, we propose a foundation for a Dutch ultrasound curriculum for internists, especially for internists specialised in acute medicine, but this may be easily used for other specialties within internal medicine. It can also be incorporated into the European Training Requirements Internal Medicine that has been recently published.10 Furthermore, we describe the necessary steps to become competent in ultrasound.
FOUNDATION FOR ACUTE INTERNAL MEDICINE ULTRASOUND CURRICULUM
We suggest core applications for internists treating acutely ill patients in the Emergency Department (ED) or the ward. These suggestions are based on international guidelines for the development of ultrasound curricula in emergency medicine (see table 2).
Key issues include:
1. general ultrasound knowledge, 2. choosing core applications, 3. integrating PoCUS into clinical decision-making, 4. training and 5. achieving and maintaining competency.
1. General ultrasound knowledge
The novice sonographer must obtain a basic understanding of ultrasound.1,6 This includes physics and anatomy, basic ‘knobology’ (the functionality of controls on an instrument as relevant to their application; how does the machine work), image recording, knowledge of artefacts, basic principles of Doppler ultrasound, characteristics of different probes, and image interpretation.11 The operator must also be aware of limitations with ultrasound, for example, using caution in cases of inadequate image requisition or lower resolution when using handheld devices; and finally, operators must know their own limitations in skills and interpretation. The concept of PoCUS is to focus on specific, mostly yes-or-no questions for critical conditions in the acute setting.12 It is mainly used to rule in disease, and is less suited to rule out disease due to lower sensitivity than specificity for several conditions (“when you don’t see it, it might still be there”), but this may differ for each core application. For example, cardiac tamponade is safely ruled out if pericardial effusion is not observed. This is how PoCUS differs from structural comprehensive ultrasound examinations performed by radiologists or cardiologists, which include extensive and detailed organ evaluation.
Acquiring a basic understanding can be achieved using multiple educational modalities including lectures, readings, online education modules, and practical hands-on sessions. General ultrasound knowledge is a mandatory basic skill for every core application.
2. Core and enhanced applications
PoCUS can be divided into diagnostic or procedural applications.1,6 Diagnostic applications can be single area (for example, assessment of the kidneys for hydronephrosis) or combined areas (for example, Rapid Ultrasound in Shock including ultrasound of the heart, the inferior vena cava, and signs for deep vein thrombosis).13 Examples of procedural applications are ultrasoundguided paracentesis and venous access. It is important to determine what applications will be core applications and meet the needs of the local practice. These core applications can be complemented with a variety of specialty applications depending on individual preferences and local needs. Core applications should be relatively easy to learn, rapid to perform, be frequently encountered, and preferably have a binary yes/no question. It is relevant to know the specific diagnostic performance of ultrasound for each core application. We believe the following core applications are most useful (table 2) for internists who provide care for acute medically ill patients at the emergency department (ED) and also for those caring for acutely deteriorating patients on the ward:
Inferior vena cava (IVC)
Determination of the IVC diameter and the IVC collapsibility index reflects right atrial pressure, and can be used as a surrogate marker for central venous pressure (CVP).14-16 A high caval index (collapse > 50% in spontaneous breathing patients during inspiration) reflects a low CVP, whereas a wide diameter (> 2.5 cm) with no signs of respiratory variation reflects a high CVP. In this way, the caval index can aid in estimation of fluid balance and with repeated measurements guiding fluid management of patients with (undifferentiated) shock.17
Assessment of free fluid
This assessment requires a structured approach to look for signs of free fluid in three predefined regions:
Findings of free fluid can aid in diagnosing ascites or blood (ruptured aneurysm/extra-uterine pregnancy). Using PoCUS reduces the risk of complications from abdominal paracentesis by 68% and makes a focused aspiration of smaller amounts of free fluid possible compared with ‘blind’ paracentesis.18
Basic abdominal ultrasound
This includes renal, bladder, abdominal aorta, and gallbladder ultrasound. Acute (on chronic) kidney injury (AKI) is a common problem in general internal medicine, and although postrenal causes of AKI are infrequent and often suggested by medical history, the finding of hydronephrosis can significantly impact clinical management. Grading of hydronephrosis can be challenging, but interpreting a binary yes or no question (presence/absence of hydronephrosis) in PoCUS is relatively easy to learn with fair sensitivity (85%) and specificity (71%).19 If hydronephrosis is present, an ultrasound of the bladder should include bladder volume measurement to determine the level of urinary tract obstruction. Enhanced renal PoCUS skills may include kidney measurements and identifying signs of inflammation.
Acute abdominal pain is another main reason for ED visits. An abdominal aortic aneurysm (aorta > 3 cm maximum diameter) is an important diagnosis to be ruled out, and can be simply done with ultrasound; even non-radiologists can perform this with high diagnostic accuracy.20 The presence of cholelithiasis and signs of cholecystitis can be reliably investigated with PoCUS,21 as gallstones are seen as hyperechogenic structures with shadowing. There is a high suspicion of cholecystitis with a sonographic Murphy’s sign (abdominal tenderness from pressure of the ultrasound probe over the visualized gallbladder), gallbladder wall thickening (wall > 3 mm), and pericholecystic fluid, especially in the presence of cholelithiasis. Basic abdominal ultrasound can be enhanced with multiple specialty applications including pancreas ultrasound, liver ultrasound, bowel and appendix ultrasound, genitourinary ultrasound, or vascular ultrasound, depending on local expertise, hospital policy and individual patient needs.
Basic cardiac ultrasound
Comprehensive cardiac ultrasound can be a difficult exam, but a simplified focused cardiac ultrasound can be learned with high sensitivity and specificity for binary questions, comparable to cardiologist-performed ultrasound.22 These binary questions include looking for pericardial effusion (sensitivity 86%, specificity 86%), signs of right ventricular enlargement (sensitivity 93%, specificity 98%), and making a global assessment of the left ventricular function (normal or low, sensitivity 89%, specificity 96%). Internal medicine residents have been also able to identify left ventricular systolic dysfunction with high sensitivity and specificity (both 94%) after limited training.23 These findings can assist in the differential diagnosis of shock, for example, obstructive shock in massive pulmonary embolism and pericardial effusion/ tamponade, or cardiogenic shock in case of severely reduced left ventricular function.
Pulmonary ultrasound
Shortness of breath is a frequently encountered clinical problem with a large differential diagnosis. Lung ultrasound can identify pneumothorax, interstitial syndromes with excess interstitial fluid like pulmonary edema, pneumonia, or pleural fluid.25,26 A widely used protocol for structured lung ultrasound is the Bedside Lung Ultrasound in Emergency (BLUE) Protocol, which was published in 2008.27 In this protocol, the pleural line is reviewed, which can be seen as lung sliding with each respiration originating from the movement of the visceral and parietal pleura. The presence of lung sliding excludes a pneumothorax whereas identifying the lung point (the point where the visceral pleura separates from the parietal pleural at the margin of a pneumothorax) is pathognomonic for a pneumothorax. The pulmonary parenchyma is aerated in healthy patients which blocks ultrasound signals at the pleural line. With ultrasound, this induces a reverberation artefact of the pleural line and this is seen as repetitive horizontal lines called A-lines. When interstitial fluid is present (for instance pulmonary edema or pneumonia) these A-lines are erased by vertical, hyperechoic, well-defined comet-tail like lines, arising from the pleural line and traversing the entire screen to the bottom, called B-lines. Other findings may include an- or hypoechogenic fluid (pleural fluid) or signs of pneumonia. Lung ultrasound can assist in fluid resuscitation as emerging bilateral B-lines can indicate fluid overload/pulmonary edema.
Procedural assistance
PoCUS is widely used to guide a variety of procedures, including thoracic and abdominal paracentesis, central line placement, or venous access.
3. Clinical decision making
The aforementioned core applications can be taught in modular fashion. When these individual competences are mastered, they can be combined in the work up of various clinical presentations, including a patient with shock, shortness of breath, and acute abdominal pain.
Shock
A patient with undifferentiated shock should be assessed with the Rapid Ultrasound in Shock (RUSH) protocol.28 According to this three-part protocol, ‘the pump’, ‘the tank’ and ‘the pipes’ are assessed. ‘The pump’ represents the heart (contractility, pericardial effusion, right ventricular enlargement, and potentially chamber size); ‘the tank’ represents vascular volume and includes the IVC, lung ultrasound, and abdominal assessment for free fluid; ‘the pipes’ denote the evaluation of the large vessels for rupture or occlusion (aorta and deep venous thrombosis). Combining these three steps generally illustrates to a more specific group of shock (obstructive, distributive, hypovolemic, or cardiogenic shock).
Shortness of breath
Another example of combining these core applications is during the assessment of a patient with shortness of breath. Evaluation of cardiac function and lung ultrasound may show signs of intrapulmonary edema (B-lines) and a severely impaired ventricular function. An enlarged right ventricle and a wide IVC with absence of collapse may suggest pulmonary embolism requiring a deep vein ultrasound absolutely necessary to search for DVT.
Abdominal pain
Finally, PoCUS can be used in a patient with acute abdominal pain. A hyperdynamic heart with a small and collapsed IVC can point to a ruptured abdominal aortic aneurysm, ectopic pregnancy, or abdominal sepsis. In a patient with pain in the right upper quadrant, PoCUS may display gallstones, cholecystitis, or hydronephrosis. Lower abdominal pain can be caused by urinary retention which can be easily visualized and measured with ultrasound. To adequately interpret the PoCUS results for these clinical conditions, the operator must be aware of the different sensitivities and specificities, as well as the positive and negative predictive values for the individual core applications. These results must be combined with the clinical findings and other results.
4. Training
Each specific core application can be learned in a modular fashion. The IFEM point-of-care ultrasound curriculum guideline provides an overview of the three training steps necessary to learn PoCUS and achieving competency (table 3), namely: initial introduction, gaining experience and achieving competency. This must be complemented with a fourth step which is staying competent.
Initial introduction
The initial introduction includes a basic knowledge of ultrasonography, the details of the relevant specific application, and the trainee must demonstrate knowledge and skills under direct trainer supervision. In most countries, a variety of courses are offered, complemented with lectures, demonstrations, readings, E-learning and online teaching videos, local practical sessions, or other sources of information.
Gaining experience
This second phase requires practicing ultrasound on real patients with direct feedback from supervisors, which may be followed by image review. This can be achieved in the ED or on the ward during morning rounds and key features include: improving image acquisition, interpreting images within clinical context depending on patient characteristics and image quality, and incorporating ultrasound results into clinical decision making. The trainee should demonstrate knowledge about image quality and limitations, in cases of suboptimal images. Image review is possible after the operatorpatient encounter and even through remote real-time telemonitored ultrasound (telesonography) during the procedure. Subtle changes, however, in probe handling and movement for improving image quality are best learned hands-on with bedside supervision. Self-learning is sometimes possible if the patient undergoes additional testing, for example, a comprehensive ultrasound or computed tomography (CT) scan. The trainee may ask the patient if he/she can practice performing an ultrasound and compare the results with the results of the CT scan. Most importantly, ultrasound findings must be integrated with other clinical data and test results for optimal decision making. This often is the most difficult part of the PoCUS curriculum and trainees should check their conclusions with colleagues and other specialists. Differential diagnosis of ultrasound findings as well as pitfalls and artefacts are critical and can only be achieved through practice time and ultrasound exposure, feedback, and image review. For example, a multidisciplinary ultrasound meeting can be arranged to discuss interesting ultrasound findings. The trainee should keep track of all ultrasounds performed in a personalised portfolio with documented supervision and the possibility to review images at a later stage (see figure 1 for an example of an ultrasound portfolio with one fictional patient as used in our hospital). 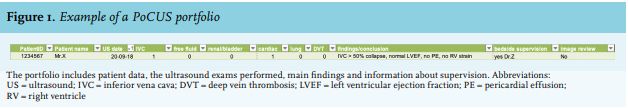
There are many online ultrasound resources (websites, YouTube tutorials) to assist with learning how to interpret images, especially those that present variations of normal findings and pathological findings. Gamification is more recent learning method, where games or game elements in non-game settings are used, ideally to increase the involvement, focus, learning, or productivity of students.29 In 2012, The Academy of Emergency Ultrasound organized the SonogGames® at the 2012 Society for Academic Emergency Medicine annual conference, to advance ultrasound education in a novel and interactive way.30 SonogGames® positively affected medical residents’ perceptions and understanding of ultrasound across clinical practice, knowledge and competence, and enthusiasm, and also added new information beyond their completed ultrasound rotations that could be incorporated into clinical practice.31 Over the past few years, ultrasound games have been developed to assist the acquisition of ultrasound knowledge and to examine skills. These games vary from very simple games such as question-based slot machines (e.g., the Abdominal Ultrasound CME Quiz developed by Philips) or image guessing games (Can U hear the U-sound? game developed by the Norwegian University of Science and Technology) to more advanced software with specifically designed probes.32,33 For example, in an underwater world game, searching for and collecting coins may improve student skills for PoCUS by increasing their spatial orientation and effective probe movements (Underwater: the ultrasound training game, Sfinx Games).34
5. Achieving and maintaining competency
The final stage is achieving competency. The trainee must demonstrate competency as assessed by supervisors for three core competencies: image acquisition, image interpretation, and clinical integration/decision-making. It is currently not known how many ultrasounds are needed to qualify as sonographer, and requirements vary, depending on organization. For radiology residents it is known that a minimum of 500 cases is required.35 ACEP requires at least 25-50 quality-reviewed exams in particular applications but also acknowledges that learning is a lifelong process with improvements beyond training, and that previously-learned psychomotor skills are often needed for new applications. Overall Emergency Ultrasound (EUS) trainees should complete a benchmark of 150-300 total EUS exams depending on the number of applications being utilised.36 The Dutch Acute Medicine taskforce on sonography organization proposes a minimum of 25 ultrasounds in each application with at least five abnormal findings. However, a recent study showed large individual variation in learning ultrasound technique for the core application IVC and 25 repetitions was inadequate to reach pre-defined competence.37 In a systematic review, Kanji et al. propose a minimum of five hours of cardiac ultrasound training with a minimum of 30 scans for binary questions, and reported better outcomes after 15 hours of training.38
Entrustable professional activity
It is time to replace the granting of competency based on the completion of a fixed number of ultrasound scans performed with a more competency-based training system. The Entrustable Professional Activity (EPA) concept has competency-based education targets to guarantee that all learners have a sufficient level of proficiency when they reach the required EPA level after training.39 The competencies should be specific, comprehensive (include knowledge, attitude, and skill), durable, trainable, measurable, related to professional activities, and connected to other competencies.40 Supervisors of trainees should be able to decide when a trainee may be entrusted to bear the responsibility to perform this professional activity, given the level of competence that is reached. This trust should be earned by demonstrating specific skills and performances with the supervisor present. We suggest an ultrasound EPA model for assessing competence including minimal requirements for each EPA level (table 4).
This model is based on a framework from Schnobrich which shows increasing levels of entrustment ranging from level 1 (not trusted to perform PoCUS even under direct supervision) to level 4 (entrusted to use PoCUS independently).41 Level 5 is more advanced and includes teaching in ultrasound which may not be reached by many trainees. Using such a model for the evaluation of every core application ensures that trainees are able to safely use PoCUS independently after reaching level 4. They are then fully aware of indications and limitations of PoCUS and are able to obtain high-quality images on almost all cases. They can also interpret most images and use them for clinical decision-making in conjunction with other clinical findings and have back-up systems for help when needed. There are several ways to demonstrate the specific skills and performances; for example, using specific PoCUS checklists for core applications like the Objective Structured Assessment of Technical Skills (OSATS). Other means of assessing competence can include images or video review with supervision, simulation-based testing including clinical decision-making, and bedside patient assessments with supervision. We have defined a minimal number of normal and abnormal ultrasound exams and OSATS for each EPA level to assist in assessing the trainee and validating the EPA level. Using EPAs with competence and assessment criteria will provide an objective and structured method for assessing PoCUS competence which includes more than becoming competent only based on a fixed number of ultrasound exams performed.
Staying competent
Finally, after achieving competence, an additional step is introduced: every doctor must maintain competency through continuous medical education. Most important is using ultrasound on a regular basis and, if needed, combining this with educational sessions or peer review. In addition to practicing ultrasound, IFEM advises at least 5-10 hours of continuing medical education credits pertaining to ultrasound activities per year.4
Quality control
Hospitals and professional organizations (for example the NIV) need to collaborate to make clear guidelines on image archiving, templates for documentation, and medicolegal policies. Images made by internists (including trainees) should also be included in the patient record and accompanied with a clear report about the clinical problem and conclusions. Saved images should be of adequate quality for peer review afterwards. Trainees should have a secured system of updating their personal portfolio with ultrasound images that does not violate privacy regulations.
CONCLUSION
Achieving and maintaining ultrasound competence is a longitudinal experience and these competences can be assessed with EPAs. EPAs are based on a variety of tools and continuous education, rather than absolute numbers of scans. A single course is insufficient to qualify a trainee as a sonographer. A well-designed curriculum is needed. Modern advances, including medical simulation and serious games can have a key role in developing skills and competences. In this article, we have proposed a foundation for an ultrasound curriculum for internists based on the current evidence and guidelines, including judging competency using EPAs.
REFERENCES